Bridging the Gap - Health Equity for all
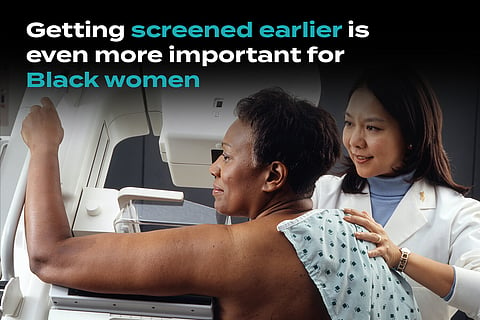
Earlier Breast Screening Could Save Black Women’s Lives
<p>Until last week, the recommendation from the US Preventive Services Taskforce (USPSTF) was that women over 50 must start getting screened for breast cancer, and those between 40 and 50 should consider doing so based on their individual circumstances, such as family history of the disease. That's now been reversed by the USPSTF so that all women should get screened at least every other year starting at 40. Increasing breast cancer rates and more evidence showing the utility of earlier screening were the driving forces behind the change.</p>
<p>However, there's another level of nuance that means some women are at an unnecessarily elevated risk of missing a diagnosis before it’s too late. Black women live with a disproportionately higher risk of dying from breast cancer, so the previous guidelines were way off the mark for them and the new ones may still not be stringent enough.</p>
<p>Research from 2023 (conducted while the USPSTF recommendation for breast cancer screening was still 50 years of age) was already critical of this given how out of touch it was with racial disparities in outcomes. The authors of one paper argued that Black women be more cautious with breast cancer screening by starting earlier at age 42 because of their elevated risk. This approach could help to reduce the racial disparities in breast cancer deaths, said the authors, who described the policy at the time as “neither fair and equitable nor optimal.”</p>
<p>“The current situation is an example of what happens when race and ethnicity are not considered in guidelines. This may pose a significant risk for greater harm to a group already at increased risk,” they continued. </p>
<p>Guidance set out by the USPSTF is based on the risk of developing breast cancer, the second most fatal cancer in American women. Groups like the American Cancer Society have previously argued in favor of lowering the recommended screening age.</p>
<figure><img alt="" height="341" src="https://cdn.storymd.com/optimized/Kq2xZkhLo5/thumbnail.jpg" width="640" />
<figcaption>Screening for Cancer. <em>Source:TheVisualMD</em></figcaption>
</figure>
<h2>Breast cancer disparities</h2>
<p>Breast cancer is the most commonly diagnosed type of cancer in women, and it is the deadliest cancer in six US states. Regular screening — even with the old guidlines — makes a huge difference in reducing the mortality risk, but there remains a stark difference in mortality rates between white and Black people.</p>
<p>The mortality rate in Black women has been steadily 40% higher than that of white women for years, and this is despite having a significantly lower incidence rate. For Black women under 50, the death rate is twice that of white women. This highlights how, for Black women especially, it's long been the case that the USPSTF guidlines have been off the mark with their risk profile, and even under the new guidlines they are still at an elevated risk.</p>
<p>According to Laurie Margolies, chief of breast imaging at the Dubin Breast Center in New York City, Black women are diagnosed younger, less likely to be diagnosed with an early form of breast cancer, and at a higher risk of dying.</p>
<p>"That's why the guidelines that say begin at age 50 are flawed and so dangerous," said Margolies, who was not involved in the study, to Medscape Medical News. "This study is really important to highlight that we're missing an opportunity to detect and treat breast cancer early in the Black population."</p>
<p>Systemic racism plays a role in why Black women may not get screened earlier or frequently enough, with bias from healthcare providers, inequities in access to and the quality of care, and mistrust within the community toward the healthcare system being examples.</p>
<h2>The findings</h2>
<p>The goal of the study was to optimize the benefits of screening by finding evidence of risk-aware starting ages in relation to race and ethnicity. The adapted screening ages were based on each group’s 10-year cumulative breast cancer-specific mortality risk. </p>
<p>The researchers looked at data on 415,277 breast cancer deaths in US female patients between 2011 and 2020. The breakdown of the total cohort was 75% white, 15% Black, 7% Hispanic, 3% Asian/Pacific Islander, and 1% American Indian or Alaska Native (AIAN). Some 115,214 women (28% of the cohort) died before age 60.</p>
<p>The old USPSTF recommendations under scrutiny in the study stated that individual women in their 40s discuss with their clinician when they should start screening, and their mass breast cancer screening recommendation for 50 and up is based on a 10-year cumulative breast cancer mortality risk of 0.329%. In the study, researchers found that Black women hit this threshold at 42; white women at 51; AIAN at 57; and Asian/Pacific Islanders at 61.</p>
<p>“The take-home message for US clinicians and health policymakers is simple. Clinicians and radiologists should consider race and ethnicity when determining the age at which breast cancer screening should begin,” said co-author Mahdi Fallah to CNN.</p>
<p>On top of earlier screening, clinicians should consider more frequent mammograms as well as alternative methods, according to the authors. </p>
<figure><img alt="" height="426" src="https://cdn.storymd.com/optimized/RA85R7i9o9/thumbnail.jpg" width="640" />
<figcaption>Breast Self-Exam. <em>Source: National Cancer Institute</em></figcaption>
</figure>
<h2>Earlier screening benefits outweigh the cons</h2>
<p>The breast density in Black women tends to be higher, making it tougher to spot cancer during a screening as well as raising the risk of the disease. They are also more likely to develop more aggressive variants such as triple-negative breast cancer.</p>
<p>An argument against earlier screening is that it raises the risk of a false-positive, meaning more wasteful testing along with deep emotional stress. The authors countered that this risk is outweighed by the benefits of earlier detection, emphasizing that equity — not equality — should be pursued by policymakers.</p>
<p>Equity in this context means that everyone is provided with screening according to their risk level instead of a blanket answer of women 50 (or even 40) and up. “We believe that a fair and risk-adapted screening program may also be associated with optimized resource allocation,” they added.</p>
<h2>StoryMD’s Breast Cancer Journey Library</h2>
<p>If you have been diagnosed with breast cancer or are seeking guidance on how to maximize your odds of prevention, you can find your ultimate guide in StoryMD’s Breast Cancer Journey, a dedicated multimedia library covering every detail in plain language.</p>
<p>Here, you can dig in on everything you need to know about risk factors, symptoms, screening, diagnosis, treatment, and more. Find answers to frequently asked questions, understand the role of genetics, and learn what lies ahead on your journey if you’ve received a diagnosis.</p>
<p>The StoryMD Breast Cancer Journey library was used to critical effect by Susan Tsiaras, wife of StoryMD CEO Alexander Tsiaras, on her breast cancer journey. She <a data-tabindex-counter="1" data-tabindex-value="none" href="https://storymd.com/story/Kq2Wwa9c4A-susan-s-breast-cancer-journey-part-1-storymd-health-s-technology-empowers-her-personalized-health" tabindex="-1">chronicled her incredible story </a>in an article published on the StoryMD site last week.</p>
<h2>More on Breast Cancer Diagnostics and Screening</h2><ul><li><a href="https://soulivity.storymd.com/journal/jk7g9equbm-breast-cancer-screening" target="_blank">Breast Cancer Screening: Mammography and Other Screening Tests</a></li><li><a href="https://soulivity.storymd.com/journal/9jkppl8ibm-mammography" target="_blank">Mammography: How to Prepare, What to Expect, Possible Risks</a></li><li><a href="https://soulivity.storymd.com/journal/mp9zq93f6w-cancer-disparities" target="_blank">Reducing Health Disparities to Promote Health Equity in Cancer</a></li></ul>